How Do I Know If Someone Is At The End Of Life? Recognizing The Signs
Detail Author:
- Name : Lindsey Carroll
- Username : reese.steuber
- Email : hillary.flatley@champlin.org
- Birthdate : 2007-05-28
- Address : 2401 Darryl Harbors East Trey, UT 68533
- Phone : +1-484-894-4439
- Company : Hyatt-Schiller
- Job : Broadcast Technician
- Bio : Eligendi aut facilis autem perferendis omnis. Optio et at quidem ex ullam eius ipsam. Nobis consequuntur expedita quia vel repellat.
Socials
linkedin:
- url : https://linkedin.com/in/yessenia7188
- username : yessenia7188
- bio : Quia at dolorem porro ex omnis omnis in.
- followers : 5478
- following : 512
tiktok:
- url : https://tiktok.com/@grahamy
- username : grahamy
- bio : Rerum nostrum nam aut. Sapiente aut dolores nihil quaerat.
- followers : 845
- following : 1395
Knowing when a person is nearing the end of their life can be one of the most difficult times for anyone. It brings up many feelings, and it is a time when people often feel a lot of uncertainty. You might wonder how to offer comfort, or what to expect next, so it's understandable to look for some guidance. This kind of knowledge, in a way, helps you prepare for what is ahead, offering a sense of what to do.
There are subtle shifts that happen as someone approaches their final days. These changes can be physical, like how they breathe or eat, and also emotional, showing up in their mood or how they interact with others. Understanding these signs can help you feel a bit more prepared, and perhaps, a little less alone in this very personal process, you know?
This article aims to shed some light on the various signs that might tell you someone is at the end of life. We will talk about common changes you might observe, offering some clarity during a time that can feel quite hazy. Learning about these things can, arguably, make a difference in how you support your loved one and yourself.
Table of Contents
- Recognizing Physical Changes
- Emotional and Mental Shifts
- The Role of Healthcare Professionals
- Supporting Someone at the End of Life
- When to Seek Help
- Frequently Asked Questions
Recognizing Physical Changes
As a person nears the end of their life, their body begins to slow down. This is a natural part of the process, and it shows itself in several ways. These physical changes are, in a way, the body preparing for its final rest. It's important to remember that every person's experience is unique, but there are some common signs you might observe, so.
Changes in Breathing Patterns
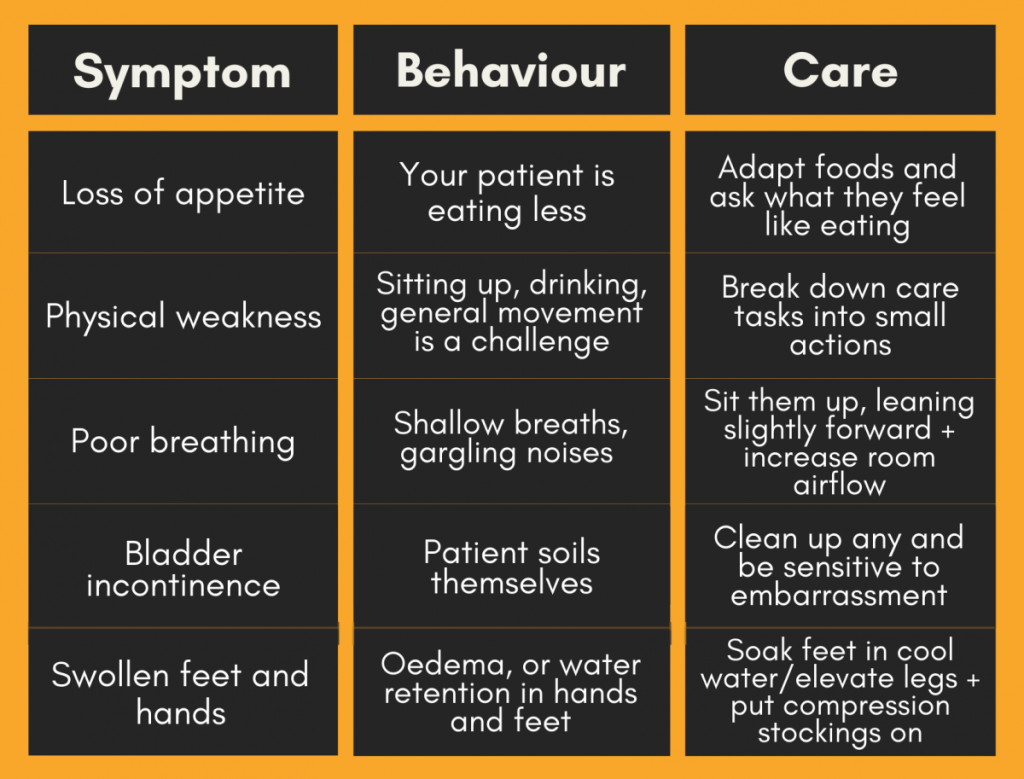
One of the most noticeable changes can be in how a person breathes. You might observe periods where their breathing becomes quick and shallow, then slows down, or even pauses for a short time before starting again. This is often called Cheyne-Stokes breathing, and it's a common sign, you know. Sometimes, there might be a gurgling sound in their throat, which can be upsetting to hear, but it typically does not cause discomfort for the person themselves, pretty much.
These breathing changes are due to the body's systems winding down. The brain's control over breathing becomes less regular. You might also notice that their breaths become more labored, like they are putting more effort into each one, or perhaps, they might seem to be breathing through their mouth more often, too it's almost.
Altered Eating and Drinking Habits
A person nearing the end of life will usually have a much smaller desire for food and drink. They might refuse meals, or only take a very small amount of liquid. This is a normal part of the process, as the body's need for energy decreases. For instance, offering sips of water or small pieces of soft food might be all they can manage, or, frankly, nothing at all.
It can be hard for family members to see someone not eat or drink, because we often connect food with comfort and care. However, forcing food or liquids can actually cause discomfort, leading to problems like choking or fluid buildup. So, it is usually better to follow their lead and offer only what they seem to want, basically.
Skin Changes
The skin can show some signs as well. You might notice that the person's hands and feet feel cool to the touch. Their skin might also look mottled, meaning it has a purplish or bluish pattern, especially on their arms and legs. This happens because the circulation of blood slows down and moves away from the extremities to focus on vital organs, so.
Their skin might also appear pale or a bit waxy. This is, in a way, another sign of reduced blood flow. Keeping them warm with blankets can offer comfort, but remember, the coolness of their skin is a body process, not necessarily a sign they feel cold, you know, in that case.
Reduced Body Temperature
As the body slows, its ability to regulate temperature can change. You might find that the person's body temperature drops, making them feel cool to the touch. This is a common occurrence. It is not usually a sign that they are feeling cold themselves, but rather a reflection of the body's metabolic rate decreasing, so.
You can still provide warmth and comfort with light blankets or by adjusting the room temperature slightly. However, trying to raise their body temperature significantly is not typically recommended, as it might cause more discomfort than help, apparently.
Sleepiness and Unresponsiveness
A person at the end of life will often spend more and more time sleeping or drifting in and out of awareness. They might become difficult to wake up, or they may not respond to voices or touch in the way they used to. This is a natural consequence of the body conserving energy and the brain receiving less oxygen, a bit.
Even if they seem unresponsive, it is often believed that hearing is one of the last senses to go. So, continuing to talk to them, holding their hand, or playing gentle music can still offer comfort and a sense of presence, pretty much. Just a little presence can mean a lot, to be honest.
Less Control Over Bodily Functions
As the body's muscles relax and its systems wind down, a person might lose control over their bladder and bowels. This is a common and expected part of the dying process. It is not something to be ashamed of or embarrassed about, obviously.
Using absorbent pads or briefs can help manage this, ensuring the person stays clean and comfortable. Healthcare professionals, like a doctor of osteopathic medicine (D.O.), who is a fully trained and licensed doctor, can offer guidance on how to manage these situations with dignity and care, you know. A doctor of osteopathic medicine graduates from a U.S. school, so they have a lot of practical experience.
Emotional and Mental Shifts
Beyond the physical changes, there are often shifts in a person's emotional state and mental awareness. These can be just as important to recognize as the physical signs, offering a different kind of insight into what they are experiencing. These shifts are, in a way, a reflection of their inner journey, you know.
Withdrawal and Detachment
Many people at the end of life will begin to withdraw from the world around them. They might show less interest in conversations, hobbies, or even the presence of loved ones. This is a natural process where they are letting go and turning their focus inward. It is not a rejection of you, but rather a necessary step for them, arguably.
This withdrawal can feel upsetting for family and friends, who might want to connect more. However, respecting their need for quiet and space is important. Simply being present in the room, holding a hand, or offering a gentle touch can be enough, sometimes. It's about being there, just a little.
Restlessness or Agitation
Some people might experience periods of restlessness or agitation. They might pick at their bedclothes, try to get out of bed, or seem distressed. This can be caused by various factors, including changes in metabolism, pain, or simply the body's natural processes. It's a common, if challenging, part of the experience, as a matter of fact.
Healthcare professionals can help identify the cause of the restlessness and suggest ways to manage it, perhaps with medication or by adjusting their environment. Creating a calm and peaceful setting, with soft lighting and quiet sounds, can sometimes help ease agitation, pretty much.
Vision-like Experiences
It is not uncommon for people nearing the end of life to talk about seeing people who are not there, or to describe places they seem to visit. These can be comforting experiences for them, often involving deceased loved ones or familiar, peaceful settings. These are sometimes called "visions" or "dreams," and they are quite real to the person experiencing them, you know.
It is generally best to acknowledge these experiences without trying to correct or dismiss them. For instance, you might say, "It sounds like you're seeing someone special," or "That sounds like a peaceful place." These experiences are, in a way, a part of their unique journey, so.
Changes in Communication
Communication patterns often change significantly. A person might speak less, or their words might become difficult to understand. They might also communicate in ways that are not verbal, like through gestures, facial expressions, or even just their presence. This is, in some respects, a shift in how they interact with the world around them.
Even if verbal communication becomes difficult, you can still connect through touch, eye contact, or simply by being near them. Reading to them, playing their favorite music, or just sitting quietly can be very meaningful ways to communicate care and presence, you know, at the end of the day.
The Role of Healthcare Professionals
During this time, the guidance of healthcare professionals is incredibly valuable. A doctor of osteopathic medicine, also known as a D.O., is a fully trained and licensed doctor who can offer a lot of support. These doctors graduate from a U.S. school, and they are equipped to help manage symptoms and provide comfort, for example.
Healthcare professionals often prescribe medications to manage symptoms like pain, nausea, or restlessness, much like they might prescribe statins to lower cholesterol and protect against heart attack and stroke for people, though statins may lead to side effects in some. The goal at the end of life is to ensure comfort and dignity, you know. They can explain what is happening, what to expect, and how to make your loved one as comfortable as possible, basically.
They can also help families understand the process and offer emotional support. Their expertise is, in a way, a steady hand during a very turbulent time. They are there to answer questions and to guide you through each step, so. It is not clear whether food with plant sterols or stanols lowers your risk of heart attack or stroke — although experts assume that foods that lower cholesterol do cut the risk. But the main point is that healthcare professionals are a vital resource.
Supporting Someone at the End of Life
Providing comfort and support during this time means focusing on the person's needs and wishes. This might involve creating a peaceful environment, ensuring they are free from pain, and simply being present. Remember that healthy cells die at a set time, and this is a natural process for the whole body, too it's almost. This understanding can help you accept the changes you observe.
You can offer comfort in many ways. This includes gentle touch, soft words, or playing calming music. Sometimes, just sitting quietly with them is enough. It is about showing your love and care in a way that feels right for both of you, you know. For instance, you might offer a cool cloth on their forehead or simply hold their hand, just a little.
It is also helpful to talk to other family members and friends about what is happening. Sharing feelings and experiences can provide mutual support. This is a journey that affects everyone involved, and supporting each other can make a big difference, you know, in some respects. Learn more about caregiving on our site.
When to Seek Help
It is always a good idea to reach out to healthcare professionals if you have questions or concerns about the changes you observe. They can provide reassurance, adjust care plans, or offer new strategies for comfort. If you are unsure about any symptom or behavior, or if you feel overwhelmed, contact them, basically.
Hospice care teams are especially skilled in supporting people at the end of life and their families. They can provide medical care, emotional support, and practical assistance. They are a wonderful resource during this period, offering specialized care and guidance, for instance. You can find more information about hospice care from organizations like the Hospice Foundation of America, naturally.
Remember, you do not have to go through this alone. There are people and resources available to help you and your loved one navigate this tender time. It is a very personal journey, but there is support to be found, you know. You might also find helpful information on this page support for caregivers, too.
Frequently Asked Questions
What are the very last signs of life?
The very last signs often include very shallow breathing, long pauses between breaths, and sometimes a complete lack of response to touch or sound. The skin might also appear mottled or bluish, especially on the hands and feet. These are usually the signs that indicate death is very near, arguably.
What are the signs of death in the next 24 hours?
In the last 24 hours, you might see more pronounced changes in breathing patterns, increased sleepiness or unresponsiveness, and a significant decrease in food and liquid intake. There might also be changes in skin color and temperature. Restlessness or agitation can also be present, sometimes, you know.
What are the 5 stages of dying?
The five stages of grief, often discussed by Elisabeth Kübler-Ross, are denial, anger, bargaining, depression, and acceptance. While these stages are about grief, they can also apply to a person facing their own death, though not everyone experiences them in the same order or even experiences all of them, basically. It's more of a framework than a strict progression, so.